Fascia: The Connective Web that Shapes Our Body
Derived from the Latin term for band, bandage, swathe, and sheath, fascia is a complex and integrated three-dimensional continuum of specialized connective tissues and cells that play a vital role in supporting body physiology, functioning, and maintaining balance. It forms a network of interwoven layers from the macro to microscopic levels, organized into epi, peri, and endo membranes throughout various tissues.
Superficial fascia is found just beneath the skin, while deep and muscular fascia envelops and supports the muscles. Fascia also encapsulates organs (visceral fascia) and protects the brain and nerves (neural fascia) within the central, peripheral, and autonomic systems. As a result, fascia acts as a potent mediator, transmitting tension, fluid dynamics, and neural impulses throughout the entire human system, contributing significantly to our overall well-being and performance. It responds to mechanical, hormonal, and psychological factors, making it a dynamic and adaptive system.
Fascia exhibits elastic, viscoelastic, and plastic properties, allowing it to respond to physical and mechanical loads and stresses. It can absorb and transmit forces, adapt to tensioning, and remodel itself based on Wolff's Law, which governs the relationship between bone architecture and mechanical load. However, with ageing, these capacities may deteriorate, particularly in deep fascia with its essential extracellular matrix of collagen, elastin, and hyaluron. Hyaluron acts as a friction-reducing fluid, facilitating smooth gliding action over muscles and adjacent fascial sheaths. Mechanical pressure, shearing, and vibrations can influence hyaluron function and fascial mobility efficiency, impacting inflammation and pain.
Pathology, disuse, or inflammation can lead to thickened or less mobile fascia, causing adhesions and dysfunction instead of lubrication. Estrogen levels also influence fascial tissue laxity and pain perception, exemplified by variations during ovulation, ACL rupture incidence, and menstrual cycles. Stress and related biochemical components, such as glucocorticoids and catecholamines, influence fibroblast activity residing in the extracellular matrix of fascia, thereby affecting the autonomic nervous system's state.
Fascia boasts extensive and diverse neural innervation, with sensory receptors distributed throughout its structure. Mechanoreceptors are specific to certain areas, like the glabrous skin over strong fascia, while free nerve endings are present throughout. This neural network further highlights the intricate and significant role that fascia plays in our body's sensory and motor responses.
In summary, fascia is not merely a passive structural component but a dynamic and responsive network that shapes our body, influences our well-being, and plays an essential role in how we experience and respond to the world around us. Understanding the complexity and adaptability of fascia opens up new avenues for optimizing our overall health and performance.
Mechanoreceptors: The Body's Sensory Sentinels
Within the human skin, encompassing both glabrous (hairless) and hairy areas, lie the intricate mechanoreceptors (MCRs)—remarkable sensors that translate mechanical stimuli like pressure, shear, tension, and vibration into neural signals. These MCRs are classified based on various factors, including encapsulation, functional properties, receptive field characteristics, adaptation rates to stimuli, and neural transmission.
The epidermis contains free nerve endings and Merkel cell neurites (MCN), while the dermis harbours Meissner's corpuscles (MC), Pacinian corpuscles (PC), and Ruffini corpuscles (RC) at different depths. MCNs predominantly conduct light touch and low-frequency vibrations with slow adaptation (SAI). RCs sense stretch, shear, proprioception, and low-frequency vibrations (SAII), while MCs detect pressure, indentation, and low-frequency vibrations (FAI). PCs are responsible for detecting high-frequency vibrations, deep pressure, and textures (FAII). MCNs and MCs have smaller receptive fields, whereas PCs and RCs have larger ones.
In essence, these receptors act as peripheral sentinels for primary somatosensory afferent fibres originating in the dorsal root ganglia. These fibres connect to the dorsal root of the spinal cord (sensory input) through the dorsal horn. The MCR input is then transmitted to the central nervous system (CNS) via three major spinal tracts: the dorsal column lemniscal pathway (DC-ML), spinocervical tract (SCT), and spinothalamic tract (STT). From there, somatosensory signals are integrated and make connections through the Thalamus into the somatosensory cortical areas I and II. Furthermore, MCRs are interconnected and integrated with proprioceptive pathways and higher centres.

The role of MCRs extends beyond sensory perception; they also play a crucial role in driving motor functions, such as muscle recruitment and output. Stimulation of cutaneous and fascial MCR receptive fields initiates a complex cascade of neural responses, activating interneurons and motor neurons to fire muscle fibres. Additionally, MCRs augment proprioceptive sense, both of which are vital for motor skill learning and performance.
Interestingly, while palmar fascia MCRs display background neural discharge or "standby status," plantar fascia MCRs exhibit no such baseline activity. They must be specifically stimulated to become activated and contribute to the body's intricate sensory and motor systems.
The role of MCRs extends beyond sensory perception; they also play a crucial role in driving motor functions, such as muscle recruitment and output. Stimulation of cutaneous and fascial MCR receptive fields initiates a complex cascade of neural responses, activating interneurons and motor neurons to fire muscle fibres. Additionally, MCRs augment proprioceptive sense, both of which are vital for motor skill learning and performance.
Interestingly, while palmar fascia MCRs display background neural discharge or "standby status," plantar fascia MCRs exhibit no such baseline activity. They must be specifically stimulated to become activated and contribute to the body's intricate sensory and motor systems.
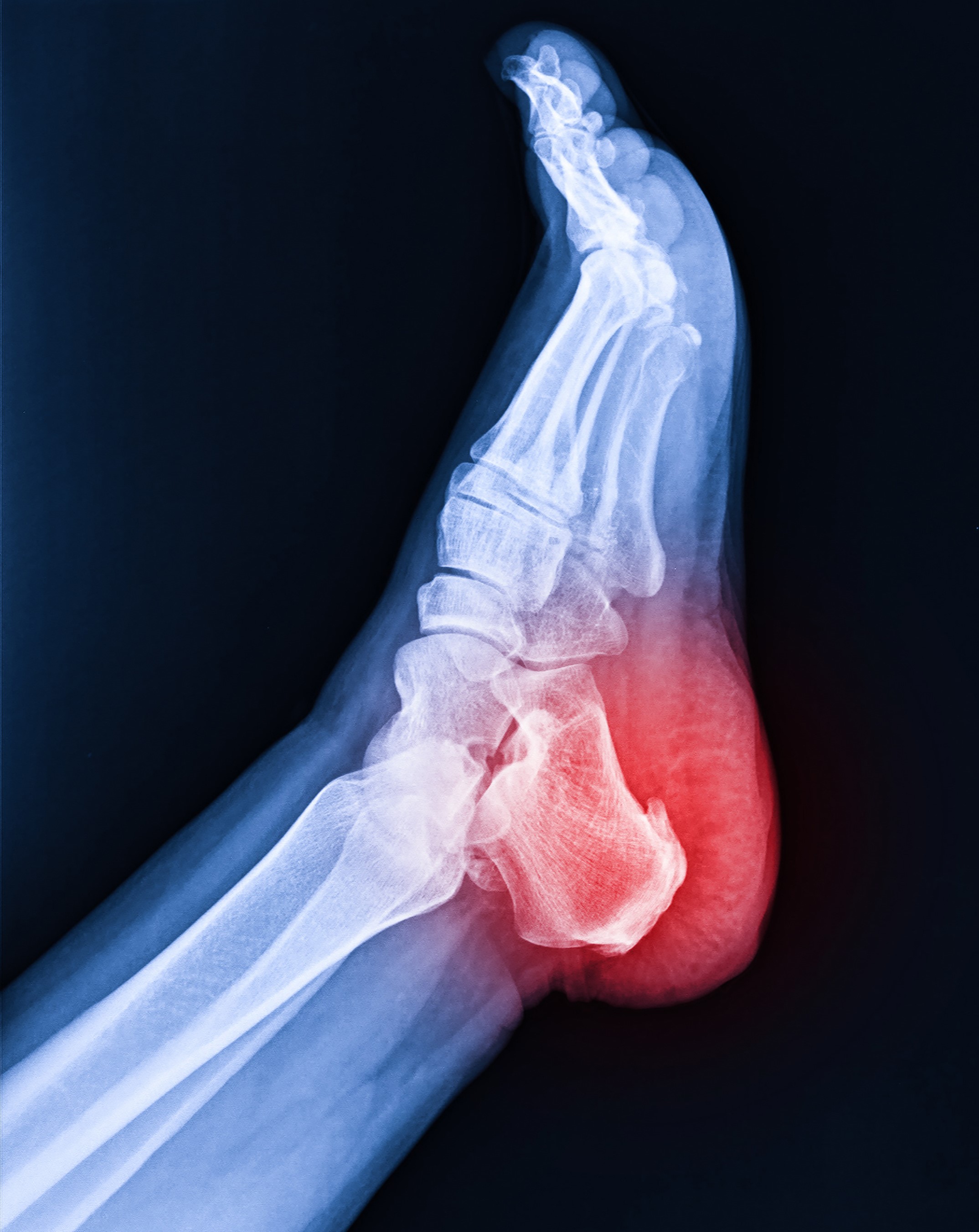
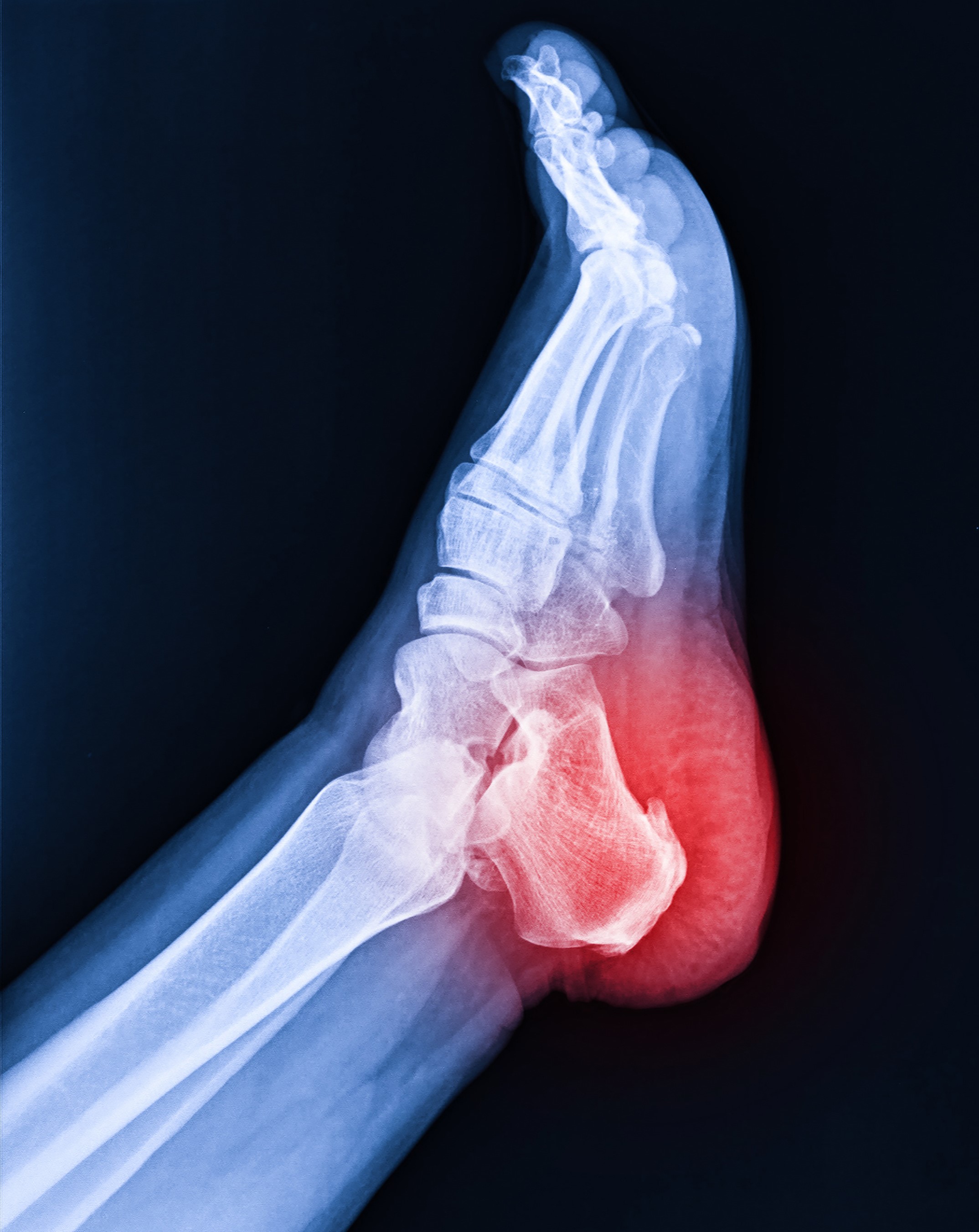
Plantar Fascia: The Key Player in Human Movement
The plantar fascia stands out as one of the strongest and most vital components within the fascial system. It plays a crucial role in managing ground reaction forces (GRF), providing a solid foundation for both static and dynamic human movement. Beyond its role in supporting movement, the plantar fascia transmits initial somatosensory input to the central nervous system (CNS) and fascial network. Additionally, it generates propulsive forces and efficiently conveys them throughout the entire fascial system.
Originating from the plantar calcaneal tuberosity, the plantar fascia extends through the medial longitudinal arch and inserts extensively across the proximal phalangeal bases, connecting with the plantar plate and plantar skin through fascial extensions. This robust structure is richly innervated by the four types of mechanoreceptors (MCRs), endowing it with crucial proprioceptive and motor coordination input.
Phylogenetically, the plantar fascia shares similarities with the tendo Achilles. It consists of two layers—the superficial and deep layers—divided into three bands: medial, central, and lateral, with connections to intrinsic foot musculature. The thickness of the plantar fascia remains fairly constant at approximately 3-4mm with age, but it may thicken in individuals with diabetes or tighten in cases of Plantar Fasciitis, often associated with increased tension in the Achilles tendon.
Plantar fascia pain may not solely originate from the foot; it can also be referred from the spine or be influenced by weak gluteal muscles, tensor fascia lata, or quadriceps' ability to respond to ground reaction forces. The plantar fascia demonstrates continuity with the fascia of the lower limb, trunk, neck, head, and internal organs through the visceral fascia. This interconnectedness allows for the fascial chain networks, commonly referred to as "from toe to tongue."
As the "first responder" to ground reaction forces, the plantar fascia stages the transmission of neural impulses and interprets mechanical signals. These responses trigger subsequent CNS reactions and motor execution, orchestrating coordination, balance, and movements. This seamless interplay between the plantar fascia, nervous system, and musculature is often described as "biotensegrity," reflecting the importance of the fascial network's integrity in supporting our body's overall function and movement abilities.
Plantar Fascia: The Key Player in Human Movement
The plantar fascia stands out as one of the strongest and most vital components within the fascial system. It plays a crucial role in managing ground reaction forces (GRF), providing a solid foundation for both static and dynamic human movement.
Beyond its role in supporting movement, the plantar fascia transmits initial somatosensory input to the central nervous system (CNS) and fascial network.
Additionally, it generates propulsive forces and efficiently conveys them throughout the entire fascial system.
Originating from the plantar calcaneal tuberosity, the plantar fascia extends through the medial longitudinal arch and inserts extensively across the proximal phalangeal bases, connecting with the plantar plate and plantar skin through fascial extensions. This robust structure is richly innervated by the four types of mechanoreceptors (MCRs), endowing it with crucial proprioceptive and motor coordination input.
Phylogenetically, the plantar fascia shares similarities with the tendo Achilles. It consists of two layers—the superficial and deep layers—divided into three bands: medial, central, and lateral, with connections to intrinsic foot musculature. The thickness of the plantar fascia remains fairly constant at approximately 3-4mm with age, but it may thicken in individuals with diabetes or tighten in cases of Plantar Fasciitis, often associated with increased tension in the Achilles tendon.
Plantar fascia pain may not solely originate from the foot; it can also be referred from the spine or be influenced by weak gluteal muscles, tensor fascia lata, or quadriceps' ability to respond to ground reaction forces. The plantar fascia demonstrates continuity with the fascia of the lower limb, trunk, neck, head, and internal organs through the visceral fascia. This interconnectedness allows for the fascial chain networks, commonly referred to as "from toe to tongue."
As the "first responder" to ground reaction forces, the plantar fascia stages the transmission of neural impulses and interprets mechanical signals. These responses trigger subsequent CNS reactions and motor execution, orchestrating coordination, balance, and movements. This seamless interplay between the plantar fascia, nervous system, and musculature is often described as "biotensegrity," reflecting the importance of the fascial network's integrity in supporting our body's overall function and movement abilities.
Fascial Dysfunction: Unraveling the Root of Musculoskeletal Issues
Musculoskeletal dysfunction (MSD) and myofascial pain (MFP) represent the primary reasons for seeking therapy interventions. Within this context, fascia and the embedded mechanoreceptors (MCRs) play a pivotal role in resolving symptoms and devising preventative strategies.
Optimal fascial condition and function are vital to maintaining the smooth operation of the fascial system (FS). When disruptions occur, it can adversely affect various FS functions, such as lubricating tissues, ensuring movement fluidity, supplying nutrients, and managing tension and compression around muscles, joints, and organs. Mechanotransduction, the process of converting mechanical stimuli into biochemical and neural responses, comes into play here. Forces stimulate cellular activity, potentially altering the gene expression of fibroblasts (cells present in fascia) and modifying the extracellular matrix. Repeated non-optimal stimulation of these fibroblasts might lead to inflammatory changes or precursors, impacting force transmission and the gliding of fascia necessary for normal musculoskeletal action and organ functioning. Consequently, unhealthy functioning fascia and MCRs can disrupt the entire musculoskeletal system and visceral functioning, contributing to pain and loss of function.
Moreover, as part of the natural aging process, oxidative changes occur within the fascia, resulting in stiffening of the fascial system and subsequent loss of force generation capacity, range of motion, and balance in the musculoskeletal system and viscera. This aging-related histological transformation can exacerbate musculoskeletal issues and imbalances.
Addressing fascial dysfunction is of utmost importance in treating and preventing musculoskeletal problems. By optimizing the condition and function of fascia and its embedded MCRs, we can unlock the potential for healthy functioning in the musculoskeletal system and support overall well-being. Therapeutic interventions that consider the fascial system as an essential component can pave the way for more effective and lasting outcomes.


